Preterm birth is defined as a delivery that occurs before 37 weeks of pregnancy. One in nine babies in the United States is born prematurely.
At Brigham and Women’s Hospital (BWH), we provide highly specialized care for preterm birth, including prevention in women at high risk for preterm birth or recurrent preterm birth and strategies to minimize complications in babies born prematurely. Our Preterm Birth Clinic features a multidisciplinary team of experts, including maternal-fetal medicine (high-risk pregnancy) specialists, gynecologic surgeons, and radiologists who also work closely with neonatologists (experts in the medical care of critically ill newborns) to optimize the long-term health of both mothers and babies impacted by preterm birth.
Cervical Insufficiency & Preterm Birth Video
Preterm birth affects about 7% to 10% of pregnancies, with the majority of these occurring spontaneously. Tom McElrath, MD, PhD, an attending in Maternal Fetal Medicine at Brigham and Women’s Hospital, discusses how we can identify cervical insufficiency and the treatment options available to help prevent preterm birth.
Preterm Birth Risk Assessment & Therapy Video
Up to 10% of women might be at risk for preterm birth, but we don’t always know who is at heightened risk. Tom McElrath, MD, PhD, discusses advancements in predicting high risk pregnancy, driven by research such as the work done at Brigham and Women's Hospital using the Life Codes Birth Cohort.
There are a wide range of medical and lifestyle risk factors for preterm birth. Examples include:
Babies born prior to 37 weeks have a higher risk of short- and long-term complications. The risk of complications increases the earlier the delivery. Depending on the maturity of the baby’s lungs at delivery, breathing and respiratory issues may occur.
Other issues may include:
Mothers of babies born prematurely also can experience anxiety, depression, and other emotional conditions.
Preconception evaluation and planning with an experienced high-risk pregnancy team is very important for women who want to become pregnant and have a prior history of preterm birth, including spontaneous preterm birth and preterm birth caused by other medical conditions. Steps can be taken prior to conception to prevent repeat preterm birth and plan for close monitoring during pregnancy.
A variety of medical and surgical approaches are available to prevent preterm birth and reduce risks of complications from preterm birth.
Maternal steroid administration includes two intramuscular injections of betamethasone 24 hours apart to accelerate the baby’s lung development (administered from 24 weeks to 34 weeks) and provide benefits to the baby’s other developing systems.
Magnesium sulfate infusion to the mother reduces the severity and risk of cerebral palsy associated with preterm newborn babies (administered from 24 to 32 weeks).
Medications that stop contractions (tocolytics) are helpful when receiving the course of steroid injections over 48 hours, but they are not recommended for long-term use during pregnancy.
Vaginal progesterone is helpful in pregnancies with a short cervix and high risk of preterm delivery.
Intramuscular progesterone is a proven therapy for the prevention of recurrent preterm birth.
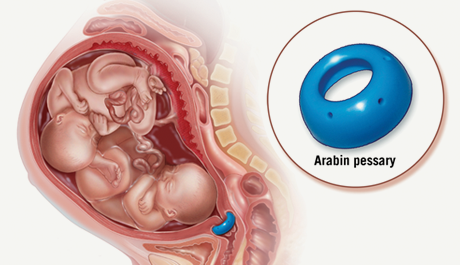
Pessary – This device is a soft, flexible ring that is placed inside of the mother’s vagina by her obstetric care provider to help prevent preterm labor in those patients who are at higher risk, including those with a shorter cervix.
Cerclage – placement of an encompassing suture around the cervix may be appropriate for some women who have a history of a prior mid pregnancy loss, or if during a current pregnancy ultrasound surveillance or physical exam indicates notable shortening or opening of the cervix. Placement of a history, ultrasound or exam indicated cerclage occurs in an operating room. The cervix is visualized with a speculum placed in the vagina and a nonabsorbent suture is placed in “purse string” fashion around the cervix. Women typically return home the same day with continued follow-up in the high risk clinic.
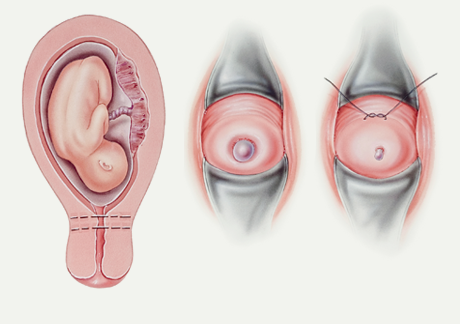
Laparoscopic abdominal cerclage – Laparoscopic abdominal cerclage is a minimally invasive procedure that is also designed to provide support at the cervical opening to the uterus. It is ideally performed before pregnancy for women who have experienced more than one cervical complication in prior pregnancy. Laparoscopic abdominal cerclage is suitable for women with prior failed vaginal cerclage or a short cervix that is ineligible for vaginal cerclage.
Laparoscopic abdominal cerclage offers a faster recovery, reduced pain and discomfort, and less blood loss compared with traditional abdominal cerclage. Patients are typically able to return home the same day of the procedure and are able to return to normal daily activities one week following the procedure. Patients can be simultaneously treated for uterine fibroids and other coexisting conditions using minimally invasive approaches.
If you have a prior history of preterm birth or have other risk factors for premature delivery, we believe that you should have access to the latest treatments provided by a team that employs a compassionate, caring, and patient-centered approach to prenatal care.
In the Preterm Birth Clinic, our expert team of maternal-fetal medicine specialists, gynecologic surgeons, and radiologists have cared for thousands of families at risk for preterm birth. We offer highly advanced medical and surgical preventative therapies and a friendly, supportive, and understanding team dedicated to your care and the care of your baby. We also work closely with many of the nation’s leading neonatologists in the Department of Pediatrics to ensure the best possible short- and long-term outcomes for preterm babies and their families.
To schedule an appointment or to learn more about our services, please contact us at (617) 732-4840.
Brigham and Women’s Hospital
CWN-3
75 Francis Street
Boston, MA 02115
Thomas F. McElrath, MD, PhD
Division of Maternal-Fetal Medicine
Jon I. Einarsson, MD, MPH
Division of Minimally Invasive Gynecology
For over a century, a leader in patient care, medical education and research, with expertise in virtually every specialty of medicine and surgery.
About BWH